Shivaprasad Khened,
Director, Nehru Science Centre, Mumbai
The story of the ‘accidental’ discovery of penicillin has been frequently told and this story has transcended across countries. Even in India, most of us, including the school children, are familiar with the story of Alexander Fleming and his serendipitous discovery of penicillin. The accidental discovery of Penicillin won Fleming and two other scientists, Ernst Boris Chain and Sir Howard Walter Florey, the coveted Nobel Prize in Physiology or Medicine for the year 1945, "for their discovery of penicillin and its curative effect in various infectious diseases." Our understanding that infectious diseases are caused by microbes - bacteria and other microorganisms - came about thanks to the research work of Louis Pasteur and Robert Koch, who explained the nature of the infectious diseases and the connection that exists between them and the disease-causing bacteria and other microorganisms. This profound understanding opened research opportunities for scientists to advance medicine, which could help in the prevention and treatment of an important group of diseases that are caused by bacteria and other microorganisms.
Penicillin and other antibiotics and vaccines developed over the past few decades, which have saved millions of lives, owe their genesis to the fundamental understanding of the nature of the microbial diseases. The story of the accidental discovery of the penicillin (antibiotics) and its benefits for humankind is now pervasive. But then the saga of antibiotics including how scientists and engineers toiled hard to mass-produce this wonder discovery - penicillin - is less known. What is even lesser-known part of the antibiotics story is that, Alexander Fleming had also predicted the rise of Superbugs - microbes, which will, over time, become immune to antibiotics and may lead to fall of the wonder drug, penicillin (antibiotics). In a talk recorded by the BBC in 1945, Fleming himself had highlighted the dangers of improper use of penicillin. He had said, ‘If the dose is too small, the microbes will not be killed and there is a danger that they will be educated to resist penicillin’. He added, ‘we might then have someone who has a simple sore throat treating himself inadequately with penicillin and educating his microbes to resist the drug. These educated microbes could then be passed on to his best friend who might get pneumonia, for which…penicillin would do no good’. Fleming added, in this case, ‘the first man through thoughtless use of penicillin would be morally responsible for the death of his best friend’. Fleming’s prophetic statement is turning out to be true in modern days.
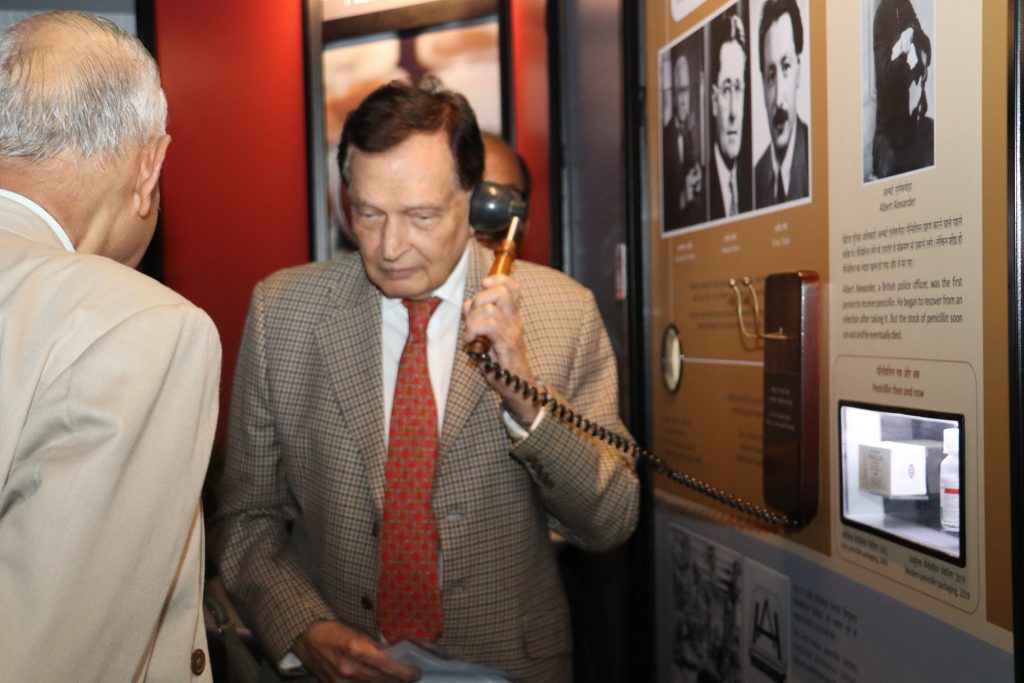
Fleming’s statement summarises the significance of what has now become a global health menace - The Antimicrobial and Antibacterial Resistance - AMR and ABR - which may eventually lead to disastrous consequences and make penicillin - the life-saving drug - completely ineffective and helpless. It is, therefore, time for all of us, the global community, to stand unitedly in addressing this global menace and for this, the first step is to create a much-needed awareness among the general public about this problem. It is in recognition of this necessity that an exhibition ‘Superbugs: The End of Antibiotics?’ has been curated and developed jointly by the National Council of Science Museums (NCSM), Ministry of Culture, Government of India, the Science Museum, Group, London, with support from the Wellcome Trust (UK) and the Indian Council of Medical Research (ICMR). This exhibition was opened by two distinguished scientists Padma Vibhushan, Prof Man Mohan Sharma, Emeritus Professor, Institute of Chemical Technology ( formerly UDCT) and eminent Physician, Padma Bhushan, Dr Farukh Udwadia in the presence of Mr. Crispin Simon, British Deputy High Commissioner for Western India and Ms. Helen Jones, Director, Global Engagement & Strategy, Science Museum Group, UK and several other dignitaries both from India and UK including a large number of students, on the 18th of December at the Nehru Science Centre. One of the important features of the exhibition is that it has several original historical objects, which narrate the story of the raise and fall of penicillin and these objects have been beautifully blended in the thoughtfully curated exhibition. The exhibition also contains large number of models, which are interactive and completely engaging. An artistically created giant model of a Superbug - made of a large number of hyper sized medicine pills - antibiotics, injectables, microbes etc. welcomes the visitors to foretell what the consequences of superbugs could be for humankind, if timely interventions are not made. An antique-looking telephone earpiece, belonging to Fleming’s era, when picked from its cradle, plays out the original voice of Alexander Fleming, where he prophetically talks of the problems of antibiotic resistance.
The Superbugs exhibition has been divided into three sections: Microscopic, Human and Global. Microscopic Section explores the hidden world of bacteria. Be it their size or characteristics, evolution of superbugs or history of antibiotics; the exhibits of this section will take you on a journey in which the visitor can zoom into the world of microbes, explore the touchscreen multimedia to understand how bacteria evolve into superbugs or flip a digital e-book to know the brief history of antibiotics.
The Human Section showcases several stories, specifically from India, of how different stakeholders of Indian society are reaching out to combat the challenge of antibacterial resistance. When antibiotics stop working, lives are put at risk. People catch infections that can’t be treated. Hospitals find it difficult to keep the spread of bacteria under control. Farmers can’t treat their animals when they become ill. Our environment poses several risks of spreading ABR in humans and animals. This section highlights how Doctors, Patients, Scientists, Researchers, Nurses, Campaigners, Pharmacists, Farmers all need to work in tandem to cope up with this problem.
Bacteria are without borders and can travel further and faster around the world than we do. Moving through our bodies, food and water systems, Superbugs on a farm in one country can spread to hospitals on the other side of the planet. The Global Sectionexplores the global initiatives in search of new antibiotics or alternate ways to combat the menace and the initiatives to create awareness on the issue. This travelling exhibition, a joint Indo-UK initiative, expressly designed and developed for the purpose of creating awareness on AMR, was first presented at the National Science Centre, Delhi, from where it has now traveled to our Centre. It will be on display for a period of two months at the Nehru Science Centre and will conclude on the 16th, February 2020. From here it will travel to Visvesvaraya Museum, Bangalore and then to Birla Industrial and Technological Museum, Kolkata.
Superbugs are those evolved microbes, which have become immune and resistant to most of the antibiotics and other medical interventions resulting in a major global health crisis. The superbugs mostly fall under AMR. The gravity of the AMR menace is a cause for concern for everyone of us and it needs collective global efforts to address this problem. AMR is an ability of microorganisms (bacteria, virus, fungi, parasites) to overcome the effects of antimicrobials (antibiotics, antivirals, antifungal, antiparasitic agents). Antibacterial Resistance (ABR) is of equal global concern that refers to the ability of bacteria to overcome the effect of antibiotics and continue to grow rapidly. While all types of AMR are concerning, ABR is currently posing the most serious health threat, particularly for India, with serious political and economic implications. The World Health Organisation (WHO) has stated that AMR is a global public health security concern, which needs to be urgently addressed. This issue has been reiterated by the WHO in numerous World Health Assembly (WHA) resolutions.
India is one of the countries which faces the highest-burden of microbial (bacterial) infections. As per the ICMR estimates, an estimated 410,000 children aged five years or less die from pneumonia in India annually; with pneumonia alone accounting for almost 25% of all child deaths. ICMR further estimates that crude mortality from infectious diseases in India today is 417 per 100,000 persons. Therefore, the impact of AMR is likely to be higher in the Indian setting and one way to try and address this issue is to create awareness and understanding of the issue of AMR. It is hoped that the Superbugs exhibition, helps in taking the message of AMR to all the stakeholders, particularly the students who visit our science centre in large numbers.
India carries one of the largest burdens of drug-resistant pathogens worldwide and therefore the Ministry of Health & Family Welfare (MoHFW) has identified AMR as one of the top ten priorities for the ministry’s collaborative work with the WHO. The AMR is also prioritized under the Global Health Security Agenda (GHSA), in which India is one of the contributing countries. The Indian National Health Policy, 2017, identifies antimicrobial resistance as a problem and calls for effective action to address this menace. It calls for a rapid standardization of guidelines regarding antibiotic use, limiting the use of antibiotics as over-the-counter medications, banning or restricting the use of antibiotics as growth promoters in animal livestock, and pharmacology vigilance including auditing prescription and antibiotic usage in the hospital and community. The emergence of AMR is not only limited to the older and more frequently used classes of drugs ( antibiotics) but there has also been a rapid increase in resistance to the newer and more expensive drugs. The ICMR finding shows that there is an increased rate of AMR, across multiple pathogens of clinical importance at the national scale. For example, according to ICMR, in 2008, based on the available data about 29% of isolates of Staphylococcus aureus were methicillin-resistant, and by 2014, this had risen to 47%. Therefore the AMR issue has emerged as a major challenge in hospitalized patients as well as in the community. In contrast, in countries that have established effective antibiotic measures and infection prevention and control programs, the proportion of methicillin-resistant Staphylococcus aureus (MRSA) isolates have been decreasing. India was the largest consumer of antibiotics for human health. However, the per capita consumption of antibiotics in India (10.7 units per capita) is lower than that seen in many other countries (22 units per capita in the USA).
Penicillin and other antibiotics have saved millions of lives and have been considered as the greatest of boon the humankind could get from scientific research. The saga of antibiotics- Penicillin - is an extraordinary episode of scientific history that heralded unprecedented international cooperation and collaboration among scientists, engineers and pharmaceutical companies, particularly between England and the United States. It all began on that eventful morning of Sept. 28, 1928, when Professor of bacteriology, Alexander Fleming, had cut short his vacation and returned back to London, hoping to help his colleague. Fleming was already working on Staphylococcus bacteria and had left behind some of his Staphylococcus samples, which he had cultured in some Petri dishes, before going on vacation. On his return to England he used some spare time in his laboratory sorting out Petri dishes bearing cultures of Staphylococcus. It was when Professor Merlin Pryce dropped into his lab to speak to Fleming. One of the Petri dishes, where Staphylococcus bacteria were being cultured by Fleming, caught their attention. A large colony of greenish mold had grown in the Petri dish and around this area no bacteria were found. It was a fascinating serendipity about which Fleming wrote that the bacterial colonies around the mold colony had “dissolved away.” The greenish colour fungus, which had inhibited the growth of staphylococcus bacteria, turned out to be ‘Penicillium notatum’, which was destined to herald a path-breaking future in the history of medicine.
Although Fleming had identified that the strain of Penicillium, which he had accidentally discovered, had killed a host of Gram-positive bacteria, including those that caused scarlet fever, pneumonia, gonorrhea, meningitis, and diphtheria, yet he was uncertain that penicillin could actually be cultivated for medical use. Cultivating penicillin indeed was a very difficult challenge and the small quantities that could be produced were mostly unstable and therefore Fleming was more or less convinced that penicillin would never be an important drug, for treatment of any of the bacterial infections. The penicillin, therefore, remained a laboratory curiosity for the next decade, until Sir Howard Walter Florey, Ernst Boris Chain and a team of researchers at Oxford University demonstrated the potential life-saving properties of penicillin. Unfortunately by then, the World War II had begun and England too was at war. War times made it difficult for the mass production of the Penicillin, since the priorities of the nation were completely different. But then with more and more soldiers dying of infections, which perhaps could have been avoided had there been a very large quantity of Penicillin, people started to think seriously on producing penicillin on a large scale. This was a Herculean task. The saga of mass production of penicillin is an extraordinary story of cooperation between nations (primarily UK and USA) and the undying spirit of collaboration between scientists and engineers, who took up this challenge. With several triumphs and tribulations, the combined efforts of scientists and engineers finally yielded the desired results, which led to the mass production of penicillin antibiotics by companies like Pfizer in the USA, who continue to be the leaders in this industry even today. Many of those who were behind this success story are unsung heroes, whose names have been confined to anonymity in the annals of history. This article makes an attempt to bring to light the roles of some of those unsung heroes - scientists and engineers - whose works made this possible.
The term Antibiotics was first coined by a US meteorologist, Matthew F. Maury, in 1855 in his book entitled ‘Physical Geography of the Sea and its Meteorology’. The reference of Maury to the term antibiotics however had nothing to do with the antibiotics that we now universally recognise. Maury was an enthusiastic observer of the sky and was keen on trying to understand the possibilities of existence of life in outer space. After serious observations, he was convinced that there is no possibility of life in outer space. But then he used an interesting phrase to express how he arrived at this conclusion that life does not exist in outer space. He wrote “I incline to the antibiotic hypothesis”, there was no alien life out there in space. The first medical recognition of the role of Penicillium (antibiotics) dates back to London in 1871, when Sir John Burdon Sanderson noted that thick bacterial growths quickly formed, if broth were exposed to air. But, if a mold like Penicillium grew on the surface of the broth then the bacteria would die. The current modern meaning of the term antibiotics gained momentum courtesy a French microbiologist, Pierre Vuillemin, who in 1890 defined an “antibiotic” as any substance that was “injurious to or destructive of living matter, especially microorganisms.” Sir Sanderson’s crucial observations were confirmed by another English Surgeon of eminence, Joseph Lister, who introduced carbolic acid as an antiseptic for use in operating rooms. Lister’s objective was to ensure that post-surgery bacteria must never gain entry to an operation wound, which continues to be the main cause of concern even this day. Lister recorded that samples of urine contaminated with the mold would not support the growth of bacteria. Two other French scientists, Louis Pasteur and Jules Francois Joubert, also observed the inhibition of growth in a culture of anthrax bacteria when contaminated by Penicillium. This phenomenon was named as ‘ antibiosis’ by Pasteur and Robert Koch.
The first person to come very close to discovering the antibiotics- penicillin - as we know today for its curative reasons, was a French medical student, Ernest Duchesne, who was probably born in Paris in 1874. He became fascinated with microbes in medical school, which he joined at a very young age and legend has it that Pasteur Institute rejected Duchesne’s thesis on the grounds that he was too young (23) for his medical thesis. He was, however, able to get another guide with whose guidance he worked and completed his thesis on microbial antagonism in 1897. His thesis suggested that application of penicillin fungi could alter the virulence of the microbes. Duchesne was able to concentrate his antibiotics in broth, which he used to show that it could be used to treat animals infected with bacteria. He was also successful in experimenting and growing Penicillin Glacum. But then before he could attempt any further work, fate had its own wish and Duchesne died of a pulmonary infection at a very young age (37) afflicted with TB. Most unfortunately the young doctors work of developing an effective penicillin antibiotics remained unfulfilled. Had Duchesne lived longer may be the course of antibiotics history may have been different. There were other investigators who are believed to have noticed the effects of penicillin before Fleming, but then it was only Fleming who could finally manage to discover what we now call penicillin the antibiotics.
Fleming, even before his serendipitous discovery of the staphylococcal colonies on his Petri dish, had been working for years on bacterial infections and in 1921, he had observed that nasal mucus and tears could prevent the growth of bacteria. He also discovered that nasal mucus and tears contained an active agent, which he named lysosome, an enzyme that dissolves bacterial colonies. It is perhaps this experience of Fleming, which helped him with that accidental discovery of penicillin on that historic day in September, 1928. But then from where did the Penicillium colony come from, which had inhibited the growth of his microbes the staphylococcus? When Fleming tested all their cultures for antibiotic-producing strains, he was able to find only one strain, which was identical to the fungus that had already contaminated his petri dish. Fleming identified the contaminant as a strain of Penicillium and he found that it killed a host of Gram-positive bacteria, including those that caused scarlet fever, pneumonia, gonorrhea, meningitis, and diphtheria. Fleming with the help of his colleagues tried to isolate pure penicillin from the mold. But then he observed that the pure penicillin is an unstable compound and therefore extremely difficult to cultivate and purify penicillin. Even those small quantities, which they could cultivate were unstable. All of these experiments convinced Fleming that penicillin would never be an important antibiotic for the treatment of bacterial infections. Therefore for the next decade, there was not much progress in harvesting the antibacterial properties of penicillin and it remained only a laboratory curiosity, until an Australian British, Sir Howard Florey and a team of researchers at Oxford University demonstrated its potential life-saving properties. By then the WWII had begun and the British were a part of this bloody war.
As the war progressed the fatalities of soldiers increased substantially and a large number of deaths happened because of infections suffered due to battle injuries. By then the therapeutic effects of the new found penicillin against bacterial infections were known but the quantity of the penicillin produced during this time was not even sufficient to cure one single adult patient. This compelled the British Government in 1941, to seek the help of their war ally the US in solving the problem of mass-producing penicillin. In response to the calls made by the British government four chemical and pharmaceutical companies in the US, including Pfizer, who were eventual winners in the race, responded to the British call thus plunging into race different companies to mass-produce the world’s first antibiotics drug. One of the pioneers who made mass production of penicillin possible was a lady American Chemical Engineer Margaret Hutchinson Rousseau.
Margaret Hutchinson Rousseau was an innovative chemical engineer who is credited to have designed the first commercial penicillin plant using a process called the Deep Tank Fermentation process. This new process enabled scientists to produce large quantities of the life-saving drug. She is also credited with other accomplishments, which include developing high-octane gasoline. She is also the first woman to join the American Institute of Chemical Engineers (AIChE). Margaret Hutchinson, while working at E.B. Badger company, was involved in designing production plants, such as those used to generate synthetic rubber. It was here that she met here future husband Mr Rousseau. Margaret Hutchinson’s modified deep tank fermentation process helped scientists to produce penicillin on a large scale. As a result, she created the first commercial penicillin plant, the use of which helped people gain access to this much-needed drug. Around the same time, a group of researchers including Dorothy Crowfoot Hodgkin discovered the structure of penicillin, which accentuated the manufacturing process of penicillin. Thanks in part to Ms. Rousseau’s work, the advancements made in penicillin production saved many lives, both in the 1940s and today.
The Pfizer company was one of those who decided to take the gamble of using the new deep tank fermentation process. In September 1943, they purchased one of the old Ice Plant in a nearby building and rebuilt this facility into the world’s first large-scale penicillin factory. On March 1, 1944 Pfizer’s penicillin plant opened. It contained fourteen 7,500- gallon tanks. Very soon Pfizer started producing five times more penicillin then originally estimated, making Pfizer the leading supplier of the drug. This was the war time and most of the penicillin that was produced by Pfizer plant on Marcy Avenue in Brooklyn, was transported in service of the Allied forces.
The success of the mass production of the penicillin goes to the marvel of chemical engineering which was practiced at Pfizer and other chemical companies in US. The production of penicillin began with a sterile culture of the penicillin mold, which was then propagated in stages from litre flasks to leading up to larger tanks of 200 gallons “seed” tanks. From this stage, the culture was transferred to huge fermenter tanks containing microbe fodder, chiefly corn steep liquor, milk sugar, salts, and minerals. The mold was allowed to grow for two to four days. The next and trickiest part of the process was extracting penicillin from the broth, since penicillin constituted a small fragment of just four parts drug per 10,000 parts broth. The extracted material was then purified and bottled in sterile rooms as extreme care had to be taken in these last steps to avoid contamination. After the bottles were filled, the penicillin moved through a freezing apparatus and then into a vacuum drier which dehydrated the drug. The final product helped the allied forces to decisively win World War II.
Alexander Fleming and his co-discoverers - Ernst Boris Chain and Sir Howard Walter Florey - truly deserve the credit for their discovery of penicillin and other antibiotics. But their monumental discovery would have remained only in the laboratory shelf if not for the extraordinary contributions by other scientists and chemical engineers who helped translate their lab discovery into the development of deep tank fermentation which eventually turned out to be a game-changer. Unfortunately after serving humankind for several decades and saving millions of lives, this very wonder drug penicillin and antibiotics have now lost their potency largely due to human neglect and misuse. It is therefore time that we rethink on what has led us to this stage of helplessness and it is hoped that the Superbugs exhibition will help in creating that much-needed awareness on the proper use of the antibiotics and hope that the global community comes together once again to address this issue of Superbugs. It was science that saved millions and it is hoped that science clubbed with society will once again help the wonder drug antibiotics to claim that pinnacle position that it once had climbed.
Jai Vigyan.
Courtesy: https://khened.blogspot.com/